Disclaimer: I am not an epidemiologist, but there is an interesting potentially important pattern in the data that seems worth understanding.
World healthcare authorities appear to be primarily shifting towards Social Distancing. However, there is potential to pursue a different strategy in the medium term that exploits a vulnerability of this disease: the 5 day incubation time is much longer than a 4 hour detection time. This vulnerability is real—it has proved exploitable at scale in South Korea and in China outside of Hubei.
Exploiting this vulnerability requires:
- A sufficient capacity of rapid tests be available. Sufficient here is perhaps 30 times the number of true new cases per day based on South Korea’s testing rate.
- The capacity to rapidly trace the contacts of confirmed positive cases. This is both highly labor intensive and absurdly cheap compared to shutting down the economy.
- Effective quarantining of positive and suspect cases. This could be in home, with the quarantine extended to the entire family. It could also be done in a hotel (… which are pretty empty these days), or in a hospital.
Where Test/Trace/Quarantine are working, the number of cases/day have declined empirically. Furthermore, this appears to be a radically superior strategy where it can be deployed. I’ll review the evidence, discuss the other strategies and their consequences, and then discuss what can be done.
Evidence for Test/Trace/Quarantine
The TTQ strategy works when it effectively catches a 1 – 1 / reproduction number fraction of cases. The reproduction number is not precisely known although discovering 90% of cases seems likely effective and 50% of cases seems likely ineffective based on public data.
How do you know what fraction of cases are detected? A crude measure can be formed by comparing detected cases / mortality across different countries. Anyone who dies from pneumonia these days should be tested for COVID-19 so the number of deaths is a relatively trustworthy statistic. If we suppose the ratio of true cases to mortality is fixed, then the ratio of observed cases to mortality allows us to estimate the fraction of detected cases. For example, if the true ratio between infections and fatalities is 100 while we observe 30, then the detection rate is 30%.
There are many caveats to this analysis (see below). Nevertheless, this ratio seems to provide real information which is useful in thinking about the future. Drawing data from the Johns Hopkins COVID-19 time series, and plotting we see:
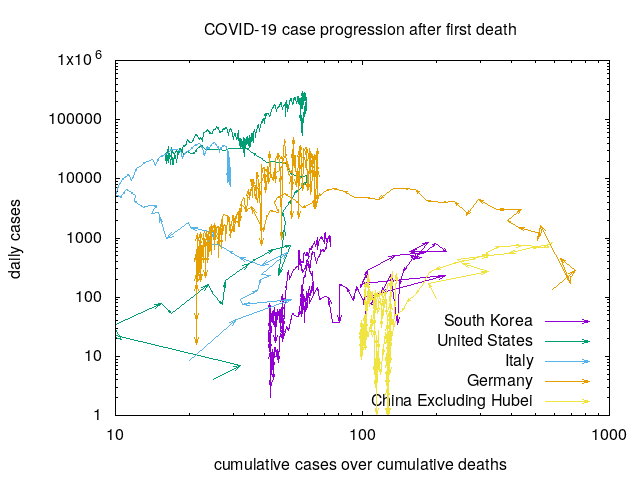
The arrows here represent the progression of time by days with time starting at the first recorded death. The X axis here is the ratio between cumulative observed cases and cumulative observed deaths. Countries that are able and willing to test widely have progressions on the right while those that are unable or unwilling to test widely are on the left. Note here that the X axis is on a log scale allowing us to see small variations in the ratio when the ratio is small and large variations in the ratio when the ratio is large.
The Y axis here is the number of cases/day. For a country to engage in effective Test/Trace/Quarantine, it must effectively test, which the X axis is measuring. Intuitively, we expect countries that test effectively to follow up with Trace and Quarantine, and we expect this to result in a reduced number of cases per day. This is exactly what is observed. Note that we again use a log scale for the Y axis due to the enormous differences in numbers.
There are several things you can read from this graph that make sense when you consider the dynamics.
- China excluding Hubei and South Korea had outbreaks which did not exceed the hospital capacity since the arrows start moving up and then loop back down around a 1% fatality rate.
- The United States has a growing outbreak and a growing testing capacity. Comparing with China-excluding-Hubei and South Korea’s outbreak, only a 1/4-1/10th fraction of the cases are likely detected. Can the United States expand capacity fast enough to keep up with the growth of the epidemic?
- Looking at Italy, you can see evidence of an overwhelmed healthcare system as the fatality rate escalates. There is also some hope here, since the effects of the Italian lockdown are possibly starting to show in the new daily cases.
- Germany is a strange case with an extremely large ratio. It looks like there is evidence that Germany is starting to control their outbreak, which is hopeful and aligned with our expectations.
The creation of this graph is fully automated and it’s easy to graph things for any country in the Johns Hopkins dataset. I created a github repository with the code. Feel free to make fun of me for using C++ as a scripting language 🙂
You can also understand some of the limitations of this graph by thinking through the statistics and generation process.
- Mortality is a delayed statistic. Apparently, it’s about a week delayed in the case of COVID-19. Given this, you expect to see the ratio generate loops when an outbreak occurs and then is controlled. South Korea and China-excluding-Hubei show this looping structure, returning to a ratio of near 100.
- Mortality is a small statistic, and a small statistic in the denominator can make the ratio unstable. When mortality is relatively low, we expect to see quite a variation. Checking each progression, you see wide ratio variations initially, particularly in the case of the United States.
- Mortality may vary from population to population. It’s almost surely dependent on the age distribution and health characteristics of the population and possibly other factors as well. Germany’s ratio is notably large here.
- Mortality is not a fixed variable, but rather dependent on the quality of care. A reasonable approximation of this is that every “critical” case dies without intensive care support. Hence, we definitely do not expect this statistic to hold up when/where the healthcare system is overwhelmed, as it is in Italy. This is also the reason why I excluded Hubei from the China data.
Lockdown
The only other strategy known to work is a “lockdown” where nearly everyone stays home nearly all the time, as first used in Hubei. This characterization is simplistic—in practice such a quarantine comes with many other measures as well. This can work very effectively—today the number of new case in Hubei is in the 10s.
The lockdown approach shuts down the economy fast and hard. Most people can’t work, so they can’t make money, so they can’t buy things, so the people who make things can’t make money, so they go broke, etc… This is strongly reflected in the stock market’s reaction to the escalating pandemic. If the lockdown approach is used for long most people and companies are destined for bankruptcy. If a lockdown approach costs 50% of GDP then a Test/Trace/Quarantine approach costing only a few% of GDP seems incredibly cheap in comparison.
The lockdown approach is also extremely intrusive. It’s akin to collective punishment in that it harms the welfare of everyone, regardless of their disease status. Many peoples daily lives fundamentally depend on moving around—for example people using dialysis.
Despite this, the lockdown approach is being taken up everywhere that cases are overwhelming or threaten to overwhelm hospitals because the alternative (next) is even worse. One advantage that a lockdown approach has is that it can be used now while the Test/Trace/Quarantine approach requires more organizing. It’s the best bad option when the Test/Trace/Quarantine capacity is exceeded or to bridge the time until it becomes available.
If/when/where Test/Trace/Quarantine becomes available, I expect it to be rapidly adopted. This new study (page 11) points out that repeated lockdowns are close to permanent lockdowns in effect.
Herd Immunity
Some countries have considered skipping measures to control the virus on the theory that the population eventually acquires enough people with individual immunity after recovery so the disease dies out. This approach invites severe consequences.
A key issue here is: How bad is the virus? The mortality rate in China excluding Hubei and South Korea is only about 1%. From this, some people appear to erroneously reason that the impact of the virus is “only” having 1% of 50% of the population die, heavily weighted towards older people. This reasoning is fundamentally flawed.
The mortality rate is not a fixed number, but rather dependent on the quality of care. In particular, because most countries have very few intensive care units, an uncontrolled epidemic effectively implies all but a vanishing fraction of sick people only benefit from home stay quality of care. How many people could die with home stay quality of care? Essentially everyone who would otherwise require intensive care at a hospital. In China, that meant 6.1% (see page 12). Given this, the sound understanding is that COVID-19 generates a factor 2-3 worse mortality than the 1918 influenza pandemic where modern healthcare might make this instead be half as bad when not overwhelmed. Note here that the fatality rate in Hubei (4.6% of known cases, which might be 3% of total cases) does not fully express how bad this would be due to the fraction of infected people remaining low and a surge of healthcare support from the rest of China.
The herd immunity approach also does not cause the disease to die out—instead it continues to linger in the population for a long time. This means that people traveling from such a country will be effectively ostracized by every country (like China or South Korea) which has effectively implemented a Test/Trace/Quarantine approach.
I’ve avoided discussing the ethics here since people making this kind of argument may not care about ethics. For everyone else it’s fair to say that letting part of the population die to keep the economy going is anathema. My overall expectation is that governments pursuing this approach are at serious risk of revolt.
Vaccine
Vaccines are extremely attractive because they are a very low cost way to end the pandemic. They are however uncertain and take time to develop and test, so they are not a viable strategy for the next few months.
What can be done?
Public health authorities are generally talking about Social Distancing. This is plausibly the best general-public message because everyone can do something to help here.
It’s also clear that healthcare workers, vaccines makers, and everyone supporting them have a critical role to play.
But, perhaps there’s a third group that can really help? Perhaps there are people who can help scale up the Test/Trace/Quarantine approach so it can be rapidly adopted? Natural questions here are:
- How can testing be scaled up rapidly—more rapidly than the disease? This question is already getting quite a bit of attention, and deservedly so.
- How can tracing be scaled up rapidly and efficiently? Hiring many people who are freshly out of work is the most obvious solution. That could make good sense given the situation. However, automated or partially automated approaches have the potential to greatly assist as well. I hesitate to mention cell phone tracking because of the potential for abuse, but can that be avoided while still gaining the potential public health benefits?
- How can quarantining be made highly precise and effective? Can you estimate the risk of infection with high precision? What support can safely be put in place to help those who are quarantined? Can we avoid the situation where the government says “you should quarantine” and “people in quarantine can’t vote”?
Some countries started this pandemic setup for relatively quick scaleup of the Test/Trace/Quarantine. Others, including the United States, seem to have been unprepared. Nevertheless, I am still holding out hope that the worst case scenarios (high mortality or months-long lockdowns) can be largely avoided as the available evidence suggests that this is certainly possible. Can we manage to get the number of true cases down (via a short lockdown if necessary) to the point where an escalating Test/Trace/Quarantine approach can take over?
Edit: I found myself remaking the graph for myself personally so I made it update hourly and added New York (where I live).
Yisong mentioned related observations from an Italian town.
A 50% drop in gdp will bring populations on its knees and governments in chaos,so no lockdowns over 3 months.Testing with immediate results (30 min.seems achieveable).
Massive testing makes tracing unn.
Tracing selfreg.Healthy people back to work without delay.Assesment of real risk for agegroups
We must start moving again!!!
I would suggest one small change on what to chart – instead of charting new daily cases – divide it by last day total cases to observe just the increase (one line change) – this way it’s better normalized regardless size of the country / magnitude of the outbreak itself
The countries that have COVID-19 under control, like South Korea, Hong Kong and Singapore, all have social distancing in addition to highly effective contact tracing, pre-emptive quarantine of close contacts and testing. The reason is that trace / quarantine / test can never be perfect. Some will inevitably slip through. Social distancing reduces the size of the outbreaks that result when these slips occur, small enough that they can be traced, quarantined and tested until they are stamped out.
It’s like fighting a wildfire. You have a firebreak (travel restrictions) and on the safe side of it you have reduced flammability as much as possible (social distancing). When fires start nevertheless, you spot them fast and put them out (trace, quarantine, test). All of these work synergistically.
The good news is that if you have all of these working well at the same time, your social distancing doesn’t have to be as extreme. Schools, restaurants, places of worship and businesses are all still open in Singapore, where I am from. There are still social distancing measures like cohorting in schools and businesses (classes + teachers or workers are split into two cohorts that don’t encounter each other, with different meal times, different arrival and dismissal, different days they work from home) or temperature checks, capacity restrictions and increased interpersonal distance at restaurants, events and places of worship, but the city hasn’t had to go to the same lockdown as it did during SARS or in other countries. The contact tracing and testing regime gives us a high degree of confidence everyone that could be infected has been tested. The social distancing is enough to give us confidence that where the above fails we can recover and stamp out the outbreak before it gets out of control.
This makes sense. A minor point is that Test/Trace/Quarantine does _not_ need to catch everything. It only needs to catch about 3 out of 4 cases to make the exponential have a negative power. To a reasonable approximation, the only thing that matters is the sign on the power…
I think having a sufficient fraction of the population wearing masks is also important. Face masks filter out some % of viral particles in the air from being breathed in. This reduces the probability of infection per contact with an infected individual. If both the infected individual and the uninfected individual are wearing masks, this will cut down effective viral particle transmission even more.
What masks do is that it effective increases the incubation time of the virus as far as transmission is concerned. It increases the average number of contacts per transmission. So if social behavior does not change, this effective increases the average amount of time before an infected individual transmits the virus to someone else. This extra time increases the probability that the infected individual will develop noticeable symptoms and get tested/quarantined.
What this does is that it will increase the fraction of infected individuals who get caught by testing before they transmit it to someone else.
The total number of transmission events is basically Total social contact events * fraction of population infected but not quarantined * probability of transmission per contact in a given block of time.
Social distancing reduces the first variable, test/quarantine reduces the second, and face masks reduce the third. As long as the product of all three variables can be kept below a threshold, the epidemic can be controlled. The problem facing us is how to keep the product below the threshold at the lowest total social cost.
What we see from this is that the later action is taken, the higher the fraction of the population is infected. Then in order to keep the total product below the threshold, we need to keep the product of the other two below an even lower threshold. This usually implies even more harsh social distancing measures. As long as the infected, non-quarantined fraction of the population is low enough, you can relax the other 2 variables somewhat and still be ok.
Federal health authorities are advising people to not use the good ones, apparently on the theory that healthcare professionals need the limited supply more. That may be true, but this paper: https://www.nejm.org/doi/full/10.1056/NEJMc2004973 suggests that a ‘use-once’ mask could be reused many times given that the viral particles die off rather quickly. Given that, it seems pretty reasonable for people to have a good mask that’s effectively reusable a number of times.
Totally agreed. South Korea does the same thing where I’m from. I don’t know why U.S.A doesn’t make people quarantined in a different space rather than their homes? How can we trust them if they are self quarantining? They should be in a hotel/motel with a limited medical personnel with police and that’s what South Korea is doing. So these people don’t infect their family members and they don’t spread to the family members’ coworkers and friends
John, use of cell phones to assist contact tracing can be done without violating privacy for most people.
You install an app on your phone. Which basically record your location/time coordinate in your own phone. Many features already require this facility. As an example, an app which automatically saves your parking location needs to keep track of your location all the time.
Now if I fall sick. My location/time history is published. If your app determines that your coordinates intersected mine, your app notifies you.
So only my privacy is compromised. Even this compromise can be reduced by removing some of the locations where I spend most time — e.g., that could be my home or my office. These high frequency locations are notified offline rather than published. For other places. it would look like a random person with covid passed by you.
How quickly can this app be made?
its not the question of how quickly the app can be made (probably a matter of 2-3 days for an MVP and a few more days to ensure good privacy protection) The key is to convince enough people to use so they can take on the privacy risk. Another step would be to make mass availability of cheap screening tests and raise the awareness/importance of knowing/admitting being infected (despite mostly light symptoms).
Great summary!
One thing to note – terminology – that 1% is not “mortality rate”. The number you are referring to is the “case fatality ratio”. (The number of deaths per person infected). It is also not a rate because there is no time factor.
A more detailed article making a similar argument: https://medium.com/@tomaspueyo/coronavirus-the-hammer-and-the-dance-be9337092b56 .
How about adding an individual risk assessment model to the app based on age, gender, and pre-existing health conditions?
Also the government should issue certificates to people that have recovered from the disease and are now immune (assuming immunity lasts – the few 2nd infections reported so far are thought by many to be erroneous). These people would then be trusted in public spaces and with vulnerable people. We need as many of those people as possible.
Some followup pointers on things happening since this came out:
(1) The PACT paper https://arxiv.org/pdf/2004.03544.pdf . (Kudos to Sham in particular for spearheading this).
(2) The CovidSafe project https://covidsafe.cs.washington.edu/ which is implementing the PACT protocols.
(3) A news report (https://abcnews.go.com/US/road-map-recovery-report-20-million-coronavirus-tests/story?id=70230097 ) on the strategy that I was peripherally involved in thanks to Glen Weyl (running https://www.pandemictesting.org/ ) and the Harvard folks (https://ethics.harvard.edu/covid-roadmap).